1801006189-long case
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 35 yr old male came to opd with chief complaints :
yellowish discoloration of eyes since 15 days ,
abdominal distenstion since 15 days
bilateral swelling of legs since 15 days ,
shortness of breath since 10 days .
HISTORY OF PRESENTING ILLNESS :
patient was apparently asymptomatic 15 days back then he developed abdominal distenstion which is insidious in onset and gradually progressive since 15 days and he has bilateral lowerlimb swelling below knee since 15 days .patient is having breathlessness for 10 days for regular household activities like using toilet, while brushing , walking within home , patient is having itching over all the body since 10 days .
patient has loss of appetite apetite since 1 week .
NO history of abdominal pain.
NO history of chest pain , palpitations, orthopnea
NO history of cough , hemoptysis .
No histroy of melena , hemetemesis .
NO history of epigastric and retrosternal burning sensation .
No history of facial puffiness , burning micturition, decreased urine output .
NO history of confusion , drowsiness.
No history of diarrhoea.
PAST HISTORY:
patient has similar complaints in the past 5 months back and he developed yellowish discoloration of eyes for 3days ,fever was high grade , continuous not associated with chills and rigor , no evening rise of temperature, he went to hospital for 1 week and symptoms subsided after a week following which he continued consuming alcohol since then (180ml per day)
NOT a known case of diabetes, hypertension, asthma , TB , CAD.
PERSONAL HISTORY:
Diet :Mixed
Appetite : decreased
Sleep :normal
Bowel and bladder : constipation is present
Addictions: patient consuming alcohol 180 ml per day since 5 yrs. Non smoker.
FAMILY HISTORY:
NO similar complaints in the family.
GENERAL EXAMINATION:
patient is conscious,coherent, cooperative and well oriented to time ,place and person moderately built and nourished.
Pallor: absent
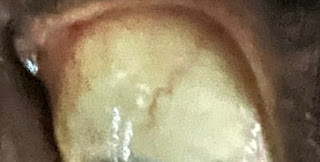
Icterus: PRESENT
cyanosis :absent
clubbing : absent
Edema : Bliateral pitting type of pedal edema is present.
lymphadenopathy:absent
VITALS:
Temperature: 98.4*C
pulse rate: 95 bpm
Respiratory rate :22cpm
SpO2: 98%
GRBS :120 mg/dl
STSTEMIC EXAMINATION
PER ABDOMEN:
INSPECTION:
Abdomen is distended.
flanks are full.
umbilicus is slit like.
skin is stretched , dilated veins present,no visible peristalsis, equal symmetrical movements in all quadrants with respiration.
Peripheral signs of chronic liver disease:
Spider naevi is absent
Palmar erythema is absent
Dupuytrens contracture is absent
Clubbing is absent
Bruises absent
Gynaecomastia absent
fetor hepaticus absent
PALPATION :
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, guarding and rigidity .
No tenderness, spleen palpable in left hypochondrium.
No organomegaly
PERCUSSION-Fluid thrill present
Shifting dullness - absent
AUSCULTATION: Bowel sounds are present .
No bruits .
CVS :
INSPECTION:
chest is symmetrical, no dialated veins , scars and sinuses seen
PALPATION: Apical impulse felt at left 5th inter coastal space medial to mid clavicular line
AUSCULTATION: S1 ,S2 heard no murmurs .
RESPIRATORY SYSTEM:
INSPECTION:
chest is symmetrical, trachea is central
PALPATION:
Trachea is normal
Bilateral chest movements are equal
PERCUSSION:
Resonant in all 9 areas
All quadrants are moving equally
AUSCULTATION:
Normal vesicular breath sounds heard.
CENTRAL NERVOUS SYSTEM:
Higher mental functions - normal memory intact
cranial nerves :Normal
sensory examination:
Normal sensations felt in all dermatomes
motor examination-
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
Normal reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
cerebellar function-Normal function.
INVESTIGATIONS :
Hemogram -
Hb- 13.2gm/dl
Total leucocyte count - 5000cells /cumm
Neutrophils - 71%
Lymphocytes -22%
RBC - 4.8 million /cumm
Electrolytes-
Sodium- 138mEq/l
Potassium - 4.4mEq/l
Chloride- 104mEq/l
Liver function tests -
Total bilirubin - 4.75mg/dl
Direct bilirubin - 2.11mg/dl
SGOT(AST) - 178 IU/L
SGPT(ALT) - 50 IU/L
ALP- 255IU/L
Total protein - 6.2 gm /dl
Albumin - 2.01 gm/dl
A:G ratio - 0.48
Ascitic tap
Appearance - clear , straw coloured
SAAG - 1.79 g/dl
Serum albumin - 2.01 g/dl
Asctic albumin - 0.22 g/dl
Ascitic fluid sugar - 166mg/dl
Ascitic fluid protein - 2.1 g/dl
Ascitic fluid amylase - 20.8 IU /L
LDH : 150IU/L
Cell count- 150 cells
Lymphocytes 90%
Neutrophils 10%
PT - 15 seconds
INR - 1.4
aPTT - prolonged
CUE:Appearance - clear
Albumin - trace
Sugars - nil
Pus cells - 2to 4
Epithelial cells - 1 to 3
RBC - nil
RFT :Blood urea - 20mg/dl
Creatinine - 0.9mg/dl
PT - 15 seconds
INR - 1.4
aPTT - prolonged
X-RAY:
USG :
Impression- liver normal size
Altered echotexture with surface irregularities present suggestive of chronic liver disease.
Mild spleenomegaly.
DIAGNOSIS
Alcoholic cirrhosis with portal hypertension.
Decompensated features are jaundice and ascites .
currently no hepatic encephalopathy or hepatorenal syndrome .
TREATMENT PLAN:
1. Fluid restriction
2. Salt restricted normal diet
3. Inj.VITAMIN K 1 ampoule in 100 ml NS OD
4. Inj.THIAMINE 1amp in 100ml NS OD
5. Inj.PAN 40mg BD
6.Inj.ZOFER 4mgTID.
7.Syrup LACTULOSE 15ml 30 mins before food TID.
8. Tab. Aldactone 50mg OD
9. Tab. LASIX 40mg BD.










Comments
Post a Comment