A 80 year old male with shortness of breath
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
CASE REPORT
A 80 year old male patient, resident of Nakrekal, farmer by occupation.
Date of history taking : 4/12/22
Date of examination : 4/12/22
CHIEF COMPLAINTS
Shortness of breath since 1 month
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 4 yrs back, then he developed SWELLING in the right leg which was progressive and pitting in nature and was diagnosed as FILARIASIS for which he did not use any medication .
Patient had h/o trauma 3 years ago in the left leg which was operated.
Since one month patient had a complaint of SHORTNESS OF BREATH which was insidious in onset, gradually progressive in nature, aggravated on walking and was not relieved on sitting and lying down and no seasonal variation.
Patient had a history of decreased urine output since 20 days and urethral structure dilation was done.
No h/o fever with chills
No h/o weight loss
No h/o burning micturition
No h/o orthopnea,palpitations
No h/o nausea,vomiting
Recently, one week ago patient developed shortness of breath which was insidious in onset and had a history of productive cough(scanty in quantity and mucoid,no foreign bodies)
PAST HISTORY
H/o previous surgery ( rod and plate fixation ) for trauma of left leg
Not a known case of diabetes , hypertension , asthma , epilepsy , tuberculosis
PERSONAL HISTORY
He is an elderly male who was farmer by occupation and stopped work since 15 yrs.
His daily routine is:Wakes up at 6:00am in the morning and Does his daily routine
Refrained from his excess physical activity
Appetite : decreased
Diet : mixed
Sleep : adequate
Bladder movements : decreased
Bowel movements are regular
Addictions - smoking in past (stopped 15 yrs ago )
Alcohol drinking in the past (stopped 1 yr ago )
FAMILY HISTORY
None of the patient’s parents, siblings, or first-degree relatives have or have had similar complaints or any significant co-morbidities.
GENERAL EXAMINATION
Patient was conscious coherent cooperative and well oriented to time place and person
He is well built and moderately nourished
Pallor - present
No icterus,cyanosis,clubbing,lymphadenopathy
VITALS
Pulse: Rate: 76 , rhythm (regular), character (normal), volume ( normal)
Peripheral pulsations [Carotid, brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis]- present
no radio radial delay
BP: 120/80 mm Hg measured on Right Upper arm in supine position
Respiratory Rate: 20 cpm
Spo2 : 96% of room air
SYSTEMIC EXAMINATION
CVS
Inspection :visible heart pulsations
Palpation:
Apex beat at 6th intercoastal space
Auscultation: S1,s2 are heard
Rhythm regularly irregular
RESPIRATORY SYSTEM
Inspection :
Chest shape normal
Breath movements -abdominal thoracic
Dysponea - present
Palpation:
Trachea -central
Percussion:
Dull note in infra axillary and infra scapular regions
Auscultation:
Coarse basal crepitations are heard
In infra axillary and infra scapular area
Wheezing heard in mammary region
Vesicular breath sounds.
ABDOMINAL EXAMINATION
Shape - Scaphoid
Tenderness - no
Free fluid - no
Liver - not palpable
Spleen- not palpable
CNS:
No focal neurological deficit
PROVISIONAL DIAGNOSIS
Dilated cardiomyopathy
Bilateral syn pneumonic effusion
With right leg filariasis ( 4yrs back)
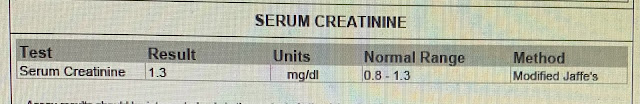
INVESTIGATIONS


X-RAY
TREATMENT
Inj. Augmentin, 1.2 gm, IV, TID
Tab. Azithra, 500 mg, OD, Per oral
Tab. Pantop, 40 mg, OD, per oral
Tab. Met xl, 25 mg, OD, per oral
Tab. Montair LC, per oral
Tab. Ecospirin, 75 mg
Tab. Ultracet, per oral, QID
Tab. Lasix, 40 mg, BD
Neb. C duolin - 4th hourly
budecort - 5th hourly
Syrup Grillinctus, 10 ml



















Comments
Post a Comment